ACA Preventive Care provides less coverage than you may think
Remember when we used to call the ACA the Patient Protection and Affordable Care Act, or PPACA? That was the name of the Senate bill that the House of Representatives ended up passing, then there was a 55-page House reconciliation bill passed by the Senate. Together, the two bills are referred to as the Affordable Care Act, or ACA.
We’re all pretty familiar with the “Affordable Care” part of the legislation. While health care and health coverage did not actually become more affordable, expanded Medicaid, premium tax credits, and cost sharing reductions did help make comprehensive health insurance coverage a reality for millions of Americans who were previously uninsured.
But what about the “Patient Protection” part – what’s that all about? Well, the law made a number of changes, in addition to the financial assistance, that make health coverage more accessible for a lot of people. For instance, insurers can no longer “discriminate” based on a person’s gender or health status; in fact, insurers offering individual and small group health plans cannot even ask medical questions on the application. The plans are also more comprehensive than before, covering the 10 essential benefits required by the federal legislation, plus additional essential benefits depending on the benchmark plan selected by each state.
Preventive Care is an Essential Benefit
One of the essential benefits that must be covered by all ACA-compliant plans—in fact, the only one mentioned in a separate provision of the law (PHS section 2713)—is preventive care. Any preventive service rated “A” or “B” by the US Preventive Services Task Force (USPSTF) must be covered up-front, prior to the deductible, with no cost sharing. That’s a pretty good benefit, one that most people seem to agree with. After all, an ounce of prevention is worth a pound of cure.
But have you ever looked at the list of services actually recommended by the US Preventive Services Task Force? It’s not as comprehensive as you might think. You can find the list here, along with the release date of each of the USPSTF’s current recommendations: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation-topics/uspstf-a-and-b-recommendations
The Recommendations are Frequently Revised
What’s interesting when looking at the list is how recent a lot of the recommendations are. In fact, only two of the recommendations were made before January of 2016, nearly six years after the ACA was signed into law. To be clear, many of the services were recommended prior to that date, but the USPSTF has revised its guidance on nearly all of it’s A or B recommended services in just that past few years.
Some Preventive Services are NOT Covered
What’s even more interesting, and probably disturbing to a lot of people, is what’s missing from the list.
For instance, an electrocardiogram, also called an ECG or EKG, as explained by The Mayo Clinic, is “a painless, noninvasive way to help diagnose many common heart problems,” including irregular heart rhythms (arrhythmias), coronary artery disease, evidence of a previous hart attack, and how well certain heart disease treatments are working. For a lot of people, the image that forms in their minds when they think of a routine physical is of a patient with electrodes taped to his or her chest and a computer readout showing their heart rhythm.

But an ECG as part of a routine physical is not recommended by the US Preventive Services Task Force. In fact, it has a rating of “D,” meaning they recommend against the procedure.
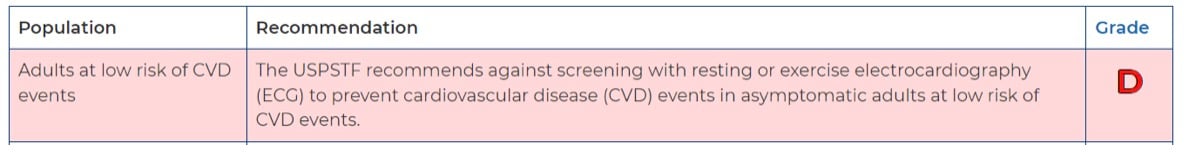 What’s more, the USPSTF does not even recommend an ECG for those at higher risk of cardiovascular disease if they are not showing symptoms, saying that “the current evidence is insufficient to assess the balance of benefits and harms of screening with resting or exercise ECG to prevent CVD events in asymptomatic adults at intermediate or high risk of CVD events.”
What’s more, the USPSTF does not even recommend an ECG for those at higher risk of cardiovascular disease if they are not showing symptoms, saying that “the current evidence is insufficient to assess the balance of benefits and harms of screening with resting or exercise ECG to prevent CVD events in asymptomatic adults at intermediate or high risk of CVD events.”
To be fair, the Mayo Clinic points out that the “American Heart Association doesn't recommend using electrocardiograms to assess adults at low risk who don't have symptoms.” And we’re not questioning the USPSTF’s or the American Heart Association’s recommendations—they’re the experts. What we are saying is that many clients, and many brokers in fact, probably do not realize this is not a covered service. And, since you certainly don’t want to misadvise clients, we thought we would let you know.
Here’s another example. A PSA test, also explained by the Mayo Clinic, is “a blood test used primarily to screen for prostate cancer. The test measures the amount of prostate-specific antigen (PSA) in your blood” and can be used as an indication of prostate cancer.”
A PSA test, however, is not a USPSTF-recommended preventive service. They give it a grade of “C” for men between ages 55 and 69 and a “D” rating (meaning they recommend against it) for men 70 years and older. Here’s what they say:
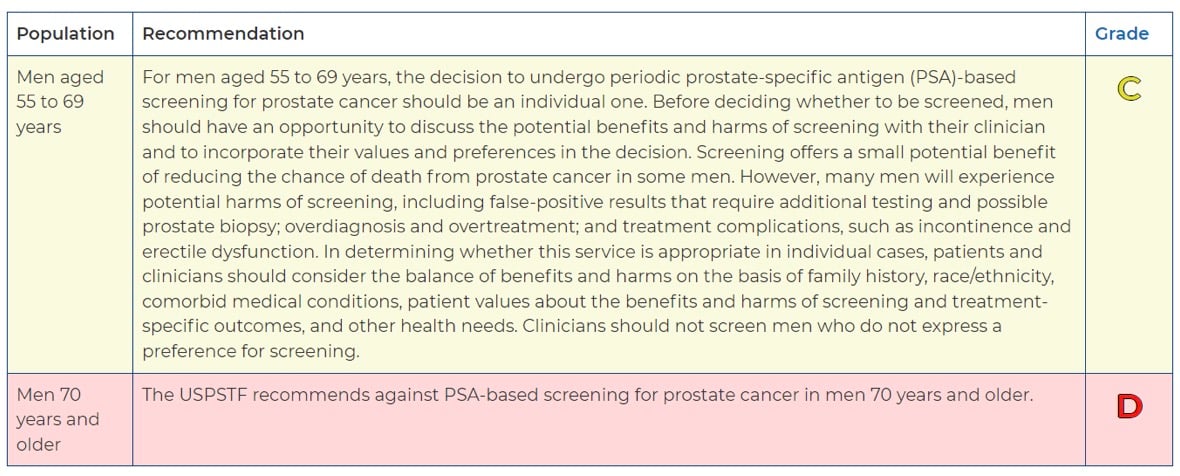
Again, we are not taking the position that PSA tests should be covered as a preventive benefit, but clients need to be aware that it is not.
These are just two examples. We could find many others. If you want information on a particular preventive service, simply do an internet search for “USPSTF” and the test or screening you are interested in. Then click on the link to the USPSTF’s website.
The Takeaway
The moral of the story here is that the Affordable Care Act, while it does make unlimited, up-front preventive care mandatory in most health plans, does not require all preventive services to be covered. There simply cannot be an annual or lifetime dollar limit on the services that are covered.
Patients may not know this and doctors may not know this, so it’s very possible that a doctor might order a test as part of what he or she considers a routine physical and the patient might receive a bill for that service. For that reason, it’s probably worth a short conversation with your clients. Let them know that preventive care is indeed covered on their health plan with no cost sharing, but not every preventive service is covered.
While some insurers might decide to cover additional preventive services, the only ones that are required to be covered are those rated “A” or “B” by the USPSTF. Again, here’s the link to that list: https://www.uspreventiveservicestaskforce.org/uspstf/recommendation-topics/uspstf-a-and-b-recommendations
Plan details are accurate as of February 15, 2023. Any changes made after this date are not addressed in this article.

